“Everybody wants a slice of the fast-growing, money-making Medicare Advantage Sector.”
Shelby Livingston
Modern Healthcare, August 20, 2018
By Stephen Tweed
One of the hottest topics of discussion over the past few months is the new policy by the Centers for Medicare and Medicaid Services (CMS) that will allow Medicare Advantage Insurance Plans to provide a range of “supplemental benefits” that are “primarily health related” to their offerings to Medicare beneficiaries.
One of the listed supplemental benefits to be offered is “In-home Support Services”. This is defined as “services to assist individuals with disabilities and/or medical conditions in performing ADLs and IADLs within the home to compensate for physical impairments, ameliorate the functional/psychological impact of injuries or health conditions, or reduce avoidable emergency and healthcare utilization. Services must be provided by individuals licenses by the state to provide personal care services, or in a manner that is otherwise consistent with state requirements.”
The letter authorizing this change, issued on April 27, 2918 by Kathryn A. Coleman, Director, Medicare Drug & Health Plan Contract Administration Group at CMS, also lists eight other supplemental services:
- Adult Day Services
- Home-Based Palliative Care
- In-Home Support Services
- Support for Caregivers of Enrollees
- Medically-approved Non-opioid Pain Management
- Stand-alone Memory Fitness Benefit
- Home & Bathroom Safety Devices and Modification
- Transportation
- Over-the-counter Benefits
What About Medicare Advantage?
 Medicare Advantage, also called “Medicare Part C” or MA plans are offered by private insurance companies approved by Medicare. These plans are an alternative to Medicare Part A & B where health care services are covered on a fee-for-services basis where hospitals, doctors, and other covered services are paid directly by CMS. Medicare Advantage Plans are paid a monthly per-member fee to cover all of the required Medicare benefits. MA Plans must cover all of the services covered by the original Medicare except Hospice services. Many Medicare Advantage Plans offer extra benefits such as dental care, eye care, and wellness programs.
Medicare Advantage, also called “Medicare Part C” or MA plans are offered by private insurance companies approved by Medicare. These plans are an alternative to Medicare Part A & B where health care services are covered on a fee-for-services basis where hospitals, doctors, and other covered services are paid directly by CMS. Medicare Advantage Plans are paid a monthly per-member fee to cover all of the required Medicare benefits. MA Plans must cover all of the services covered by the original Medicare except Hospice services. Many Medicare Advantage Plans offer extra benefits such as dental care, eye care, and wellness programs.
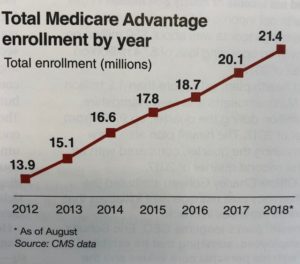
As of August 2018, 21.4 million Medicare beneficiaries were enrolled in Medicare Advantage Plans. That is up from 13.9 million covered beneficiaries in 2012. Driving that growth is the aging Baby Boomer generation who are used to having managed care plans through their employers. Seniors often get more benefits whey they choose a Medicare Advantage Plan.
These nine supplemental services authorized in April will be added benefits above and beyond the benefits that are offered to seniors enrolled in the original Medicare Fee-for-Service plan.
In 2017, there were 2,034 Medicare Advantage Plans available across the country. The top seven plans covered 75% of the market, and the top three plans serve more than half of the covered beneficiaries. The top three plans are United Healthcare, Humana, and the Blue Cross and Blue Shield companies.
What is the Potential Impact on In-Home Care?
It is way too early to tell what the impact will be on in-home care. We hear many home care owners talking about a huge inflow of new revenue. Right At Home, recently announced that it has entered into a “Preferred Partnership Arrangement” with Human. Senior Helpers just announced a new senior leadership position to forge Medicare Advantage partnerships and showcase the value of in-home care to clinicians.
As we have studied this emerging trend, there are four key questions you will need to answer to project the potential stream of new revenue from Medicare Advantage:
- Will MA Plans add In-Home Support Services to their plans? This is one of nine new benefits that will add costs, and the MA Plans will not receive any new revenue from CMS to cover thses costs.
- Will MA Plans Require these Services to be provided by a Medicare Certified Home Health Agency? MA Plans already have contracts with home health agencies to provide required home health services under Medicare. Will they simply ask these agencies to provide the non-medical supplemental services so they won’t have to vet new providers?
- If MA Plans elect to allow non-Medicare agencies to provide these services, how will they select them? Many of the home care franchise companies are developing strategies to contract with MA Plans, since they can offer wide geographic coverage. From our previous experience, we know that insurance companies what to deal with a limited number of provider organizations.
- How will you do electronic billing? Pretty much all Medicare and Medicaid services are billed electronically. What will your agency and your software vendor do to enable electronic billing. We know that Clear Care and several other home care scheduling suppliers are adding electronic billing capabilities to their software.
We were discussing this trend in one of our Home Care CEO Mastermind groups yesterday, and the consensus of the members is that we will not see a huge surge of revenue from Medicare Advantage in 2019, the first year this is offered. The long term potential for this benefit will be driven by the extent to which home care companies can show measurable results for Medicare Advantage Plans in saving money or attracting new members.
We’ll continue to monitor this trend and report to you. For a regular flow of Trendicators, short info-graphics on the top trends in home care, subscribe to our weekly newsletter, Home Care CEO Report.