By Stephen Tweed
The Centers for Medicare and Medicaid Services issued a proposed rule on Tuesday, July 1, 2014 that will redefine how home health agencies are reimbursed by Medicare for skilled intermittent home health services. Some of the highlights include:
- eliminate the requirement that physicians provide a narrative explaining the patient’s home bound status and need for skilled care
- continue the 4-year phase-in of rate re-basing that started in 2014
- implement proposed base episode rate for 2015 at $2922.76, compared to the 2014 base rate is $2869.27. While that looks like a $53.49 increase, the reality is that payment rates are actually decreased as CMS also recalibrates the case mix adjustment weights that effectively reduce those weights in the aggregate by 2.37%
- the recalibration results in some weights increasing while others decrease, primarily therapy related episodes.
- increase case mix weights by 3.75% for episodes with 0-5 therapy visits; decrease weights by 2.5% for episodes with 14-15 therapy visits; decrease weights by 5% for episodes with 20+ therapy visits; and institute gradual weight adjustments for episodes between those thresholds
- LUPA payment rates will rise 3.5% through rebasing and an additional 2.2% through the annual inflation update
- Non-routine medical supply rates are also downwardly adjusted through the re-basing by a factor of 2.82 percent
- CMS will not make any adjustment in 2015 for nominal changes in case mix weights known as “case mix creep”
- 3% Rural Add-On continues in 2015 along with the 2% rate reduction for HHAs that fail to comply with the quality data submission requirements that involve OASIS and HHCAHPS
- CMS would drop the current 13/19th visit standard for therapy reassessments and institute a requirement for a professional therapist visit/reassessment every 14 days
- CMS would institute the Value Based Purchasing program in 5-8 states. It would be a mandatory program in all the affected states. In this proposed rule, CMS is inviting comment on the VBP model including the measures, performance standards, the amount of payment that is to be placed at risk, and the states chosen for the pilot.
Public comments are permitted through August 29 (the 60th day following publication).
Let’s look at some of the trends in the industry, and how some of the new rule will propagate those trends.
 Funding the Accountable Care Act – it has been stated that the intent of the government is to fund a significant portion of the implementation of the Affordable Care Act by reducing Medicare reimbursement to providers of health care services. These cuts to home health reimbursement are part of this trend.
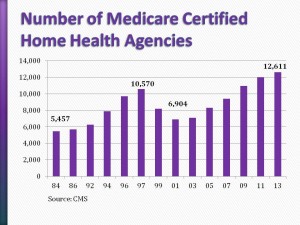
Funding the Accountable Care Act – it has been stated that the intent of the government is to fund a significant portion of the implementation of the Affordable Care Act by reducing Medicare reimbursement to providers of health care services. These cuts to home health reimbursement are part of this trend.- Too Many Agencies? – while the number of home health agencies continued to grow through 2013 – from 6,904 in 2001 to
12,611 at the end of 2013 – there are a number of industry leaders who are suggesting that CMS and some states believe there are too many certified agencies and would like to take action to reduce the numbers. - Push into Private Duty – one of the fastest growing trends has been the number of home health agencies that are refocusing on private duty home care to reduce their dependence on government payers.
What other trends are you seeing?
How will these changes affect your agency?
Add your comments below, or join our conversation in the Leading Home Care Network on LinkedIn.



